Understanding Barrett’s oesophagus metaplasia
Learn more about Barret’s oesophagus
Understanding Barrett’s oesophagus metaplasia
Learn more about Barret’s oesophagus
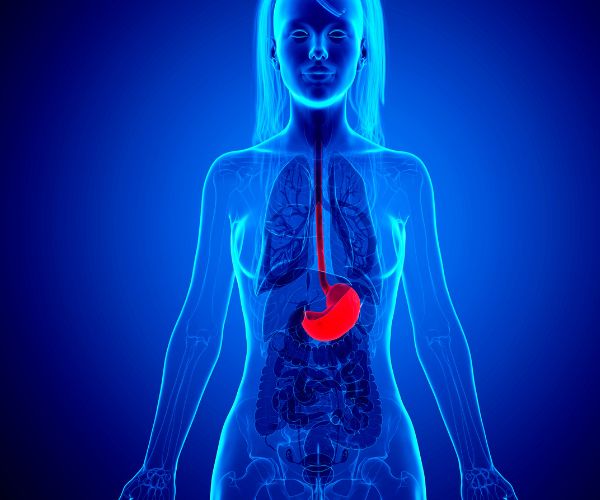
The oesophagus is a muscular tube that connects the throat to the stomach. It’s about 25 cm long in adults and plays a vital role in digestion, ensuring that the food you eat and liquids you drink reach your stomach efficiently. Barrett’s oesophagus metaplasia or Barrett’s oesophagus (BO) is a gastrointestinal condition that affects the lining of the oesophagus.
Barrett’s oesophagus happens when the cells that line the oesophagus change due to long-term exposure to stomach acid, often caused by gastroesophageal reflux disease (GORD). This process where normal cells in the oesophagus change into a different type is known as metaplasia. While it helps protect the oesophagus from acid, it also increases the risk of developing oesophageal cancer.
Common risk factors for BO include GORD, obesity, smoking, and being over the age of 50.
The oesophagus is a muscular tube that connects the throat to the stomach. It’s about 25 cm long in adults and plays a vital role in digestion, ensuring that the food you eat and liquids you drink reach your stomach efficiently. Barrett’s oesophagus metaplasia or Barrett’s oesophagus (BO) is a gastrointestinal condition that affects the lining of the oesophagus.
Barrett’s oesophagus happens when the cells that line the oesophagus change due to long-term exposure to stomach acid, often caused by gastroesophageal reflux disease (GORD). This process where normal cells in the oesophagus change into a different type is known as metaplasia. While it helps protect the oesophagus from acid, it also increases the risk of developing oesophageal cancer.
Common risk factors for BO include GORD, obesity, smoking, and being over the age of 50.

What are the types of metaplasia in Barrett’s oesophagus?
There are 2 main types of metaplasia seen in Barrett’s oesophagus:
Intestinal Metaplasia (IM)
In intestinal metaplasia, the cells lining the oesophagus change to resemble those in the intestines. This type is important because it’s linked to a higher risk of oesophageal cancer, which makes regular monitoring essential.
Gastric Metaplasia (GM)
Gastric metaplasia involves cells that resemble stomach lining cells. It doesn’t carry the same cancer risk as intestinal metaplasia, however, there is some debate about its classification as part of Barrett’s oesophagus.
What are the symptoms of Barrett’s oesophagus?
Barrett’s oesophagus often presents no specific symptoms, but it is commonly associated with symptoms of GORD. The most frequent symptoms include:
- Frequent heartburn: A burning sensation in the chest, often after eating
- Difficulty swallowing: Trouble swallowing food or a sensation of food being stuck
- Painful swallowing (odynophagia): Discomfort or pain when swallowing food
- Regurgitation: Stomach acid or food coming back up into the throat or mouth
- Chest pain: Discomfort that may mimic heart-related issues and symptoms
- Nausea and vomiting: Feeling nauseous or vomiting, sometimes with blood
- Sour taste in the mouth: This is caused by stomach acid due to acid reflux

What are the symptoms of Barrett’s oesophagus?
Barrett’s oesophagus often presents no specific symptoms, but it is commonly associated with symptoms of GORD. The most frequent symptoms include:
- Frequent heartburn: A burning sensation in the chest, often after eating
- Difficulty swallowing: Trouble swallowing food or a sensation of food being stuck
- Painful swallowing (odynophagia): Discomfort or pain when swallowing food
- Regurgitation: Stomach acid or food coming back up into the throat or mouth
- Chest pain: Discomfort that may mimic heart-related issues and symptoms
- Nausea and vomiting: Feeling nauseous or vomiting, sometimes with blood
- Sour taste in the mouth: This is caused by stomach acid due to acid reflux

What does a diagnosis of Barrett’s oesophagus involve?
To diagnose Barrett’s oesophagus, doctors typically perform an endoscopy, which involves using a small camera to examine the oesophagus. If BO is suspected, a biopsy is taken to confirm the diagnosis and to identify the type of metaplasia.
New tools like Cytosponge, a less invasive option, are also being used to detect Barrett’s oesophagus in some cases. Cytosponge is an innovative diagnostic tool consisting of a small swallowable capsule containing a sponge. Once in the stomach, the capsule dissolves, releasing the sponge that collects cells from the lining of the oesophagus as it is pulled back out through the throat.
What are the risk factors for progression to cancer?
Not everyone with Barrett’s oesophagus will develop cancer, but there is a risk, particularly for those with dysplasia. Dysplasia means that the cells have changed in a concerning way and can be classified as low-grade or high-grade. High-grade dysplasia involves severe cell abnormalities in the oesophagus and carries a greater risk of progressing to cancer.

What are the treatment options?
Though there is no cure for Barrett’s oesophagus, there are several ways to manage the condition and lower the risk of progression:
- Lifestyle changes: Avoiding foods that trigger acid reflux, maintaining a healthy weight, and stopping smoking can help reduce symptoms.
- Medications: Proton pump inhibitors (PPIs) are often prescribed to reduce stomach acid, helping to protect the linings of the oesophagus.
- Surgery: Sometimes, procedures like endoscopic resection or radiofrequency ablation may be recommended to remove or destroy abnormal tissue.
What are the current guidelines for Barrett’s oesophagus metaplasia?
Regular check-ups are key to managing Barrett’s oesophagus. How often you need monitoring depends on whether dysplasia is present:
- If there is no dysplasia, an endoscopy every 3–5 years is usually recommended
- With low-grade dysplasia, yearly endoscopies should be conducted
- For high-grade dysplasia, treatment options are discussed to prevent cancer
Barrett’s oesophagus is a condition that needs careful monitoring to catch any potential problems early. While it can increase the risk of cancer, lifestyle changes, regular check-ups, and appropriate treatment can make a big difference in reducing that risk.
Find out more about Barrett’s oesophagus metaplasia
Try to minimise your exposure to common risk factors for BO by following an active healthy lifestyle. Pay attention to maintaining a healthy body weight and avoid smoking, especially if you are over the age of 50.
If you have symptoms of gastrointestinal conditions such as GORD or suspect Barrett’s oesophagus, it’s important to talk to a healthcare professional about screening options.
Book an appointment at your nearest gastrointestinal clinic to stay informed and find out more about how you can proactively protect your oesophageal health.

Find out more about Barrett’s oesophagus metaplasia
Try to minimise your exposure to common risk factors for BO by following an active healthy lifestyle. Pay attention to maintaining a healthy body weight and avoid smoking, especially if you are over the age of 50.
If you have symptoms of gastrointestinal conditions such as GORD or suspect Barrett’s oesophagus, it’s important to talk to a healthcare professional about screening options.
Book an appointment at your nearest gastrointestinal clinic to stay informed and find out more about how you can proactively protect your oesophageal health.

FAQs
Is Barrett’s oesophagus hereditary?
While not directly inherited, having a family history of GORD or oesophageal cancer may raise your risk. Both genetics and lifestyle factors play a role.
Can Barrett’s oesophagus develop without reflux symptoms?
Yes, some people experience “silent reflux,” where stomach acid flows back without typical heartburn or discomfort, making regular screenings important.
Are there alternative ways to manage Barrett’s oesophagus?
Lifestyle changes like weight management, stress reduction, and diet adjustments can help, but they should always complement prescribed medical care.
