Everything to know about chronic gastrointestinal diseases
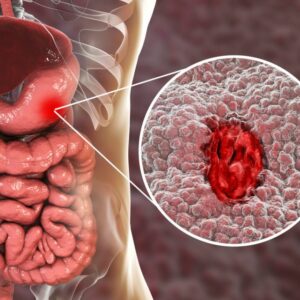
Gastrointestinal diseases have become increasingly prevalent, affecting millions of individuals worldwide. Chronic GI conditions can significantly impact one’s quality of life, making it crucial to understand their causes, symptoms, and management.
On this page, we’ll delve into some of the most common chronic gastrointestinal conditions, shedding light on their characteristics and offering insights into their treatment.
Everything to know about chronic gastrointestinal diseases
Gastrointestinal diseases have become increasingly prevalent, affecting millions of individuals worldwide. Chronic GI conditions can significantly impact one’s quality of life, making it crucial to understand their causes, symptoms, and management.
On this page, we’ll delve into some of the most common chronic gastrointestinal conditions, shedding light on their characteristics and offering insights into their treatment.

What are chronic gastrointestinal diseases?
Chronic gastrointestinal conditions are long-term conditions that affect the digestive system, causing persistent symptoms and often requiring ongoing management. These diseases encompass a wide range of conditions, each with its own set of symptoms, causes, and treatment approaches.
Chronic gastrointestinal conditions refer to a group of disorders that affect the gastrointestinal tract, including the oesophagus, stomach, intestines, and associated organs such as the liver, pancreas, and gallbladder.
Acute gastrointestinal illnesses that may resolve on their own or with short-term treatment, chronic gastrointestinal conditions can persist over time, often causing recurrent or continuous symptoms.
These conditions can range from functional disorders like irritable bowel syndrome (IBS) to inflammatory conditions such as Crohn’s disease and ulcerative colitis, as well as structural abnormalities like gastroesophageal reflux disease (GERD) and diverticulosis. Chronic GI conditions are complex and require a comprehensive approach to diagnosis and management.
What are chronic gastrointestinal diseases?
Chronic gastrointestinal conditions are long-term conditions that affect the digestive system, causing persistent symptoms and often requiring ongoing management. These diseases encompass a wide range of conditions, each with its own set of symptoms, causes, and treatment approaches.
Chronic gastrointestinal conditions refer to a group of disorders that affect the gastrointestinal tract, including the oesophagus, stomach, intestines, and associated organs such as the liver, pancreas, and gallbladder.
Acute gastrointestinal illnesses that may resolve on their own or with short-term treatment, chronic gastrointestinal conditions can persist over time, often causing recurrent or continuous symptoms.
These conditions can range from functional disorders like irritable bowel syndrome (IBS) to inflammatory conditions such as Crohn’s disease and ulcerative colitis, as well as structural abnormalities like gastroesophageal reflux disease (GERD) and diverticulosis. Chronic GI conditions are complex and require a comprehensive approach to diagnosis and management.
What are the factors of chronic gastrointestinal conditions?
Chronic gastrointestinal conditions are complex conditions that require a comprehensive approach to diagnose and manage.

Persistent symptoms
Chronic gastrointestinal conditions are characterised by ongoing or recurrent symptoms. These symptoms can include abdominal pain, bloating, diarrhoea, constipation, nausea, vomiting, and changes in bowel habits.

Impact on quality of life
The symptoms can impact the quality of life, affecting their ability to work, socialise, and engage in daily activities. Managing symptoms requires lifestyle and dietary changes, medication, or surgical interventions.

Multifactorial causes
The causes of chronic gastrointestinal illnesses tend to vary depending on the specific underlying condition which may involve a combination of factors like genetics, the environment, immunity, and lifestyle.

Need for ongoing management
Chronic gastrointestinal diseases typically require ongoing management to control symptoms, prevent complications, and improve quality of life, which requires frequent appointments and specialist interventions.
By understanding the characteristics of these diseases and implementing appropriate treatment strategies, individuals can better cope with their symptoms and lead fulfilling lives despite their diagnosis.

What are the tests that are normally done for gastrointestinal illnesses?
Testing for gastrointestinal conditions typically involves a combination of medical history assessment, physical examination, laboratory tests, imaging studies, endoscopic procedures, and sometimes, specialised tests. The specific tests recommended depend on the suspected condition and the presenting symptoms.
Healthcare providers will gather information about your symptoms, medical history, family history, medications, and lifestyle factors. A physical examination may also be conducted to assess for signs of gastrointestinal disease.
Laboratory tests play a crucial role in diagnosing gastrointestinal conditions. Blood tests such as complete blood count (CBC), liver function tests, pancreatic enzyme tests, inflammatory markers, and tests for nutritional deficiencies are commonly ordered. Stool samples may also be analysed for signs of infection, blood, inflammation markers, and occult blood.
Various imaging studies can provide valuable insights into gastrointestinal health. X-rays of the abdomen, ultrasound imaging, computed tomography (CT) scans, and magnetic resonance imaging (MRI) can help visualise the structures of the digestive system and identify abnormalities such as gallstones, inflammation, or tumours.
Endoscopic procedures, such as upper endoscopy (EGD), colonoscopy, and flexible sigmoidoscopy, allow direct visualisation of the gastrointestinal tract. These procedures can detect conditions like ulcers, polyps, inflammatory bowel disease, and colorectal cancer.
Specialised tests, including breath tests to diagnose lactose intolerance or small intestinal bacterial overgrowth (SIBO), capsule endoscopy to visualise the small intestine, and manometry to assess oesophagal function, may be utilised based on clinical suspicion.
Consulting a healthcare professional is essential to determine the appropriate tests based on individual symptoms and medical history. The results of these tests play a vital role in guiding diagnosis and planning treatment for gastrointestinal conditions.
What are the tests that are normally done for gastrointestinal illnesses?
Testing for gastrointestinal conditions typically involves a combination of medical history assessment, physical examination, laboratory tests, imaging studies, endoscopic procedures, and sometimes, specialised tests. The specific tests recommended depend on the suspected condition and the presenting symptoms.
Healthcare providers will gather information about your symptoms, medical history, family history, medications, and lifestyle factors. A physical examination may also be conducted to assess for signs of gastrointestinal disease.
Laboratory tests play a crucial role in diagnosing gastrointestinal conditions. Blood tests such as complete blood count (CBC), liver function tests, pancreatic enzyme tests, inflammatory markers, and tests for nutritional deficiencies are commonly ordered. Stool samples may also be analysed for signs of infection, blood, inflammation markers, and occult blood.
Various imaging studies can provide valuable insights into gastrointestinal health. X-rays of the abdomen, ultrasound imaging, computed tomography (CT) scans, and magnetic resonance imaging (MRI) can help visualise the structures of the digestive system and identify abnormalities such as gallstones, inflammation, or tumours.
Endoscopic procedures, such as upper endoscopy (EGD), colonoscopy, and flexible sigmoidoscopy, allow direct visualisation of the gastrointestinal tract. These procedures can detect conditions like ulcers, polyps, inflammatory bowel disease, and colorectal cancer.
Specialised tests, including breath tests to diagnose lactose intolerance or small intestinal bacterial overgrowth (SIBO), capsule endoscopy to visualise the small intestine, and manometry to assess oesophagal function, may be utilised based on clinical suspicion.
Consulting a healthcare professional is essential to determine the appropriate tests based on individual symptoms and medical history. The results of these tests play a vital role in guiding diagnosis and planning treatment for gastrointestinal conditions.

What are some chronic gastrointestinal conditions?
Inflammatory bowel disease (IBD)
This includes conditions like Crohn’s disease and ulcerative colitis, which involve chronic inflammation of the digestive tract. Symptoms may include abdominal pain, diarrhoea, rectal bleeding, weight loss, and fatigue.
Irritable bowel syndrome (IBS)
A gastrointestinal disorder characterised by abdominal pain or discomfort, bloating, and changes in bowel habits without evidence of structural or biochemical abnormalities. It can significantly impact the quality of life.
Gastroesophageal reflux disease
This is when stomach acid frequently flows back into the oesophagus, causing symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing. This can often be controlled with frequent medication.
Coeliac disease
A disorder triggered by gluten consumption, leading to damage in the small intestine; this condition can’t be cured but rather only controlled. Symptoms of coeliac disease include diarrhoea, abdominal pain, fatigue, and weight loss.
Diverticular disease
Diverticular disease involves the formation of small pouches in the colon. Complications can lead to symptoms such as abdominal pain, fever, nausea, and changes in bowel habits; this often requires surgical intervention.
Chronic pancreatitis
This is a long-term inflammation of the pancreas, which can lead to abdominal pain, weight loss, oily stools, and malabsorption of nutrients. The approach normally involves surgery, lifestyle changes, and constant medication.
Functional dyspepsia
Functional dyspepsia is characterised by persistent or recurrent upper abdominal discomfort or pain, bloating, shortness of breath, unexplained weight loss, and early satiety without any evidence of structural disease.
Gastroparesis
This condition involves delays in, or stops, the emptying and the movement of food to the stomach and is also known as gastric emptying, leading to symptoms such as nausea, vomiting, bloating, early satiety, and abdominal pain.
Gallstone disease
This involves the formation of solid particles in the gallbladder and can cause symptoms like abdominal pain after meals, vomiting, and jaundice if they obstruct the bile ducts and treatment normally involves surgical intervention.
Haemorrhoids
Haemorrhoids are swollen veins in the lower rectum or anus and are also referred to as piles, leading to symptoms such as rectal bleeding, itching, pain, and discomfort. Haemorrhoids are most often painless but can tend to bleed.
Consult a gastrointestinal specialist today
Prioritising your health is paramount, especially when it comes to recognising and addressing changes in your gastrointestinal conditions. If you notice anything unusual or persistent, seeking professional medical advice is essential.
Therefore, it’s crucial to take any abnormalities seriously and consult a healthcare professional promptly for proper evaluation and management.

Consult a gastrointestinal specialist today
Prioritising your health is paramount, especially when it comes to recognising and addressing changes in your gastrointestinal conditions. If you notice anything unusual or persistent, seeking professional medical advice is essential.
Therefore, it’s crucial to take any abnormalities seriously and consult a healthcare professional promptly for proper evaluation and management.

FAQs
What are the common symptoms of gastrointestinal (GI) diseases?
Common symptoms of gastrointestinal conditions include abdominal pain, bloating, diarrhoea, constipation, nausea, vomiting, changes in bowel habits, rectal bleeding, and unexplained weight loss. The specific symptoms vary depending on the underlying condition.
What are the treatment options for GI diseases?
Treatment for gastrointestinal conditions depends on the specific condition and may include medications, dietary modifications, lifestyle changes, and surgical interventions. Management strategies aim to control symptoms, reduce inflammation, prevent complications, and improve quality of life.
Are GI diseases curable?
The prognosis and outcomes for gastrointestinal illnesses vary depending on the specific condition, its severity, and individual factors. While some gastrointestinal illnesses can be managed effectively with treatment, achieving a cure may not always be possible for chronic or progressive conditions. However, early diagnosis, appropriate treatment, and ongoing management can help control symptoms, prevent complications, and improve the quality of life for many patients.
